Cindy Gonzalez
Nebraska Examiner
LINCOLN — One service provider billed the Nebraska Department of Health and Human Services for 32 hours of work she supposedly performed in a 24-hour day.
In another situation, the agency reportedly authorized a provider of “personal assistance services” to be paid for 118 hours of service in a typical 40-hour work week.
Yet another provider billed DHHS for client care allegedly provided on nine days when Facebook postings showed her to be traveling during that time to Indianapolis, Dallas and Phoenix.
Those and other “flagrant” instances of apparent financial abuse were identified during a probe of the DHHS’ Medicaid-funded personal assistance services program during the past fiscal year.
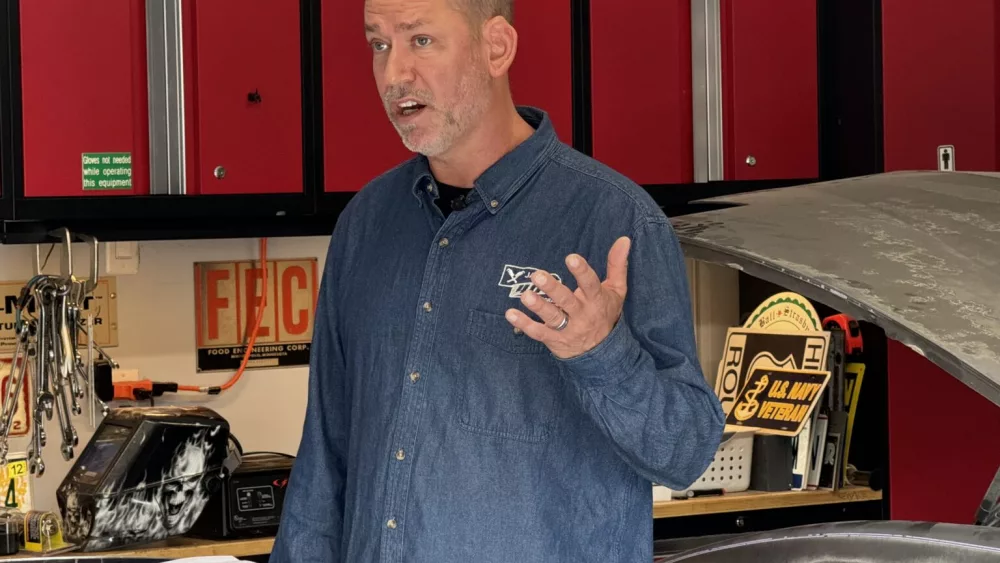
State Auditor Mike Foley said Wednesday that his auditing team found tens of thousands of dollars of questionable billings — “flagrant abuses, including suspected fraud committed by certain care providers fleecing the program to receive unearned payments.”
Based on the sample reviewed by the audit team, Foley said, an estimated annual financial loss could be up to $1.5 million.
Under guidelines for the personal assistance program, eligible Nebraskans with disabilities and chronic conditions are allowed to receive certain services such as hygiene, mobility and housekeeping from an approved care provider.
DHHS is to conduct a needs assessment of allowable services for each client. It pays providers typically about $13.52 an hour for work, and time-and-a-half for overtime.
Foley said that deficiencies have been identified for at least a decade in the program but that the latest examples convinced him it is in “desperate need of an overhaul.”
Audit findings are to be turned over to the Attorney General’s Office for further review and potential prosecution for fraud.
Steve Corsi, chief executive of DHHS, said in a statement that he is working with Foley to step up safeguards ensuring that ”taxpayer dollars are spent responsibly and funds go to supporting Nebraska’s most vulnerable individuals.”
DHHS officials were not immediately available to respond to questions. But in the auditor’s management letter, DHHS responded that the department will have recurring meetings to review deficiencies cited and to identify ways to improve.
Corrective action identified in the report: “This could include a combination of policy, business rules and technology changes as well as interim and long-term mitigation strategies.”
Foley said he trusts that Corsi will address the concerns.
DHHS currently has a system in place by which a provider’s work schedule could be tracked electronically by a GPS system and a smartphone. It’s not used in all circumstances, the audit noted.
In addition to enforcing better tracking processes, Foley said, the state should be more realistic in capping hours allowed to a provider. He said the audit revealed the likelihood that Medicaid clients were not always getting important services.
The audit covered the fiscal year ending in June 2023.
Among other examples cited by the auditing team:
- A provider claimed to have provided 87.25 hours of services in one week for three different clients despite holding down two other jobs, as a dental hygienist and a pharmacy technician. The audit team identified 101 work days in which the provider billed DHHS for services supposedly delivered during the documented work hours of her other employment.
- A provider claimed to be away on vacation on a day when her home was being targeted by an unrelated law enforcement raid. Yet she billed DHHS for 14.5 hours of service that day. The provider held other jobs as a medical assistant and a bus driver, and auditors identified 40 days in a five-month span when DHHS billings directly conflicted with hours of that other employment.
- One provider billed DHHS for personal services performed for two family members for whom she was legally responsible — a practice, the audit team said, that is prohibited by federal regulations governing the program.